Hypothyroidism
Hypothyroidism – What’s Happening
Jul 15, 2016The Butterfly That Moves Our World: Thyroid Gland
It’s the little butterfly that weights roughly 30 grams, sits in your throat and produces hormones that affect just about every cell in your body. Say hello to your thyroid gland Hypothyroidism !
No cell in our body can function properly unless the temperature is just right for the bio-chemical reactions it needs to carry out. This job is carried out by our “thermostat”, the thyroid gland. Nearly every cell in our body has ‘receptors’ for thyroid hormone, to allow they chemical it to do its job.
Thyroid hormones stimulate metabolism, help us extract nutrition and energy from food and are vital for the functioning of all other hormones in the body. When the thyroid begins to underperform, it could lead to any of the 300-plus symptoms that range from the ones we have all heard about – like feeling cold or tired, gaining weight, etc. – all the way to hives, hallucinations, unexplained muscle pains and even miscarriages.
Hypothyroidism: What’s Happening, Really?
Hypothyroidism happens when there is insufficient thyroid hormone to allow for day-to-day metabolic activities in the body. Now that we are familiar with the dramatic effects that insufficient thyroid hormone can produce, let’s get familiar with the key players in this body-wide drama.
Do bear in mind that this is not an in-depth, fully accurate explanation meant for medical students; we are focusing on the key aspects necessary for us to understand what’s happening inside us a little better.
The Key Players: Thyroid Magnum Opus Simplified
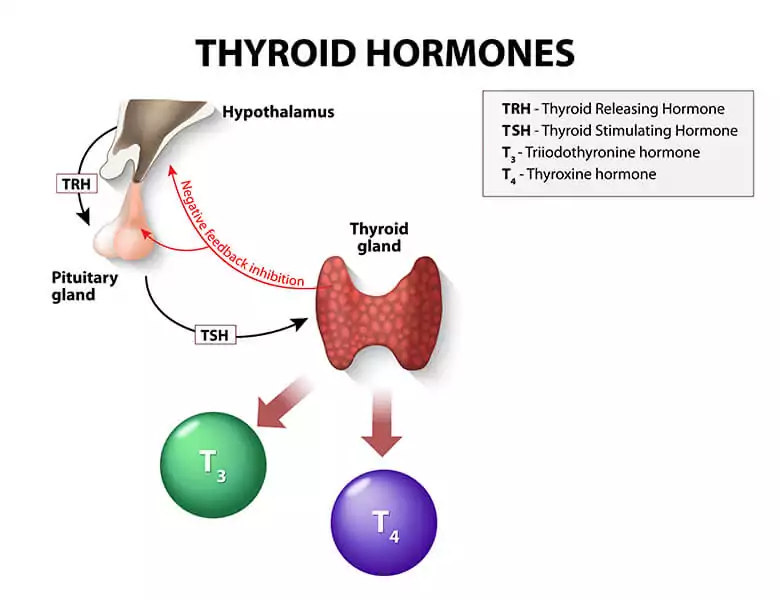
At the top of the line is our brain, the command center. Here, the blood that’s flowing through the body is constantly measured for all sorts of information, including levels of vital chemicals coursing through it, like the thyroid hormone.
When the brain finds it is below optimum, it sends a chemical messenger, aptly called Thyroid Stimulating Hormone or TSH to go “stimulate” the thyroid gland to produce more hormone. The thyroid gland then produces more of thyroxine or T4 (this is the primary thyroid hormone).
T4 is the inactive form of the thyroid hormone. It stays inactive till it reaches the peripheral tissues, where it is converted into T3, the active ‘powerhouse’ form of the hormone. This T3 then gets into the cells, which use it to power their activities.
The Sluggish (Hypo) Thyroid Of The 1900s: Missing Iodine
symptoms of iodine deficiency
Iodine is the main building block for both T3 and T4. When we are deficient in this critical mineral, this leads to ‘iodine-deficiency’ hypothyroid. This is often (though not always) characterized by a swollen or ‘goitrous’ neck.
“Iodine-deficiency” hypothyroid used to be the leading type of hypothyroid during the last century, easily fixed by giving the patient iodine. In fact, the introduction of iodized table salt into diets of whole nations was done to prevent iodine deficiency in the general population.
That said, iodine belongs to a family of minerals called halogens and chlorine, bromine and fluorine, chemicals that are often overabundant in our environment and in our bodies can “block” iodine receptors in the thyroid gland, starving it of iodine needed to manufacture T4. A small percentage of people may need to work with a trained medical practitioner, to ‘chelate’ or remove these other chemicals from the system and take supplemental iodine to support their thyroid. For most others suffering from hypothyroid symptoms, read on.
Hashimoto’s Thyroiditis: 21st Century Thyroid Disorder
The Hashimoto’s variant of thyroid disorder is the most common cause of hypothyroidism in the United States, and accounts for 90% of cases here today.
Discovered by Japanese physician Dr. Hakuro Hashimoto in 1921, Hashimoto’s Thyroiditis is an autoimmune condition that results in destruction of the thyroid gland over time.
In plain speak, for reasons yet to be discovered by science, the body’s immune system attacks its own thyroid gland, damaging it and leading to inadequate thyroid hormone production, or hypothyroidism. This kind of unexplained reaction from the immune system is called an “autoimmune” condition.
Standard Blood Tests For Thyroid Function: How They Can Mislead
When the damage to the thyroid gland is just beginning, the body compensates; the brain increases the TSH and in response, the T3 and T4 hormone levels increase, to stay within “normal” ranges in blood tests. However, even at this stage, you may begin to have symptoms . Sadly, there are so many symptoms of hypothyroidism that both patients and doctors could miss them! So unless you have a doctor who can take the time to be really thorough, the attack on the thyroid gland may simply be missed at this stage.
Progressively, as the body continues to attack itself, more thyroid tissue is destroyed and even if the brain sends more TSH to “prod” the thyroid gland, it is unable to step up T4 production in response. Blood tests at this stage will show that the person has high TSH, low T4 and often, low T3. Treatment begins and the doctor usually puts you on thyroid medication (levothyroxine) to give your body a synthetic form of the T4 on a daily basis. You begin to feel better. So far, so good.
However, to anyone who has been following the story till this point, it should be evident that this cannot be the full answer. Unless we also address the unexplained immune attack, it will continue, and eventually lead to complete destruction of the thyroid gland (called atrophic thyroiditis), considered the end-stage of Hashimoto’s thyroiditis.
The Real Curve Ball: Really Low TSH
Remember how we began this journey, with the brain as the command center , constantly monitoring the blood for all the chemicals flowing in it? Now imagine your thyroid gland, quietly doing its job, making and storing T4 in its cells for future use. Along comes an immune system that’s gone berserk and starts firing at the thyroid cells. Can you see the T4 ‘spilling’ out of the damaged storage, into the blood, saturating it? When the brain measures the blood at this point in time, it finds very high levels of T4. So what’s it going to do?
You guessed right – it mistakenly thinks that the thyroid gland is ‘making too much’ T4 (a condition known as “hyper-thyroidism”) and sends a message to the thyroid gland to cut down production. This is achieved by rapidly reducing the TSH. At this stage, the person feels symptoms of “hyperthyroidism” – such as rapid heart beat, hand tremors, palpitations, excessive sweating and anxiety.
But here is the irony. Excess thyroid hormone in the blood cannot be ‘stored’ for future use. Once it has been used up or otherwise removed from the body, our cells need T4 again. The thyroid gland, which is still under the immune attack, cannot make T4 fast enough to meet this fresh demand and voila – you have ‘hypo’ thyroid conditions again.
So patients with Hashimoto’s Hypothyroidism (which, remember, accounts for 90% of thyroid cases in the U.S. today) go through a yo-yo – from hypothyroid to hyperthyroid – as their thyroid gland in attacked by their own immune system.
So What Should You Be Testing?
In order to learn if your body is attacking its thyroid gland, you will need to measure certain thyroid antibodies in your blood. The higher they are, the greater the attack on your thyroid gland. These antibodies are called Anti-Thyroglobulin Antibody (ATG) and Anti-Thyroid Peroxidase Antibody (Anti-TPO).
Other than these, to determine how much thyroid hormone is actually available in the blood, good endocrinologists now ask labs to report TSH, Free T3 and Free T4 (the ‘free’ forms of these thyroid hormones are what are finally ‘freely available’ to the cells for metabolic functions.)
So if you have hypothyroid symptoms and we know that 9 in 10 people in the U.S. have thyroid issues of the Hashimoto’s variety today, you may want to gently suggest that your medical practitioner have these values checked for you.
Adding Insult to Injury
For a moment, let’s say this is all too confusing, too much to take in.
Could you not just ignore all this information and just take the thyroid medication? After all, hypothyroid patients used to take synthetic T4 or levothyroxine for life in the days gone by and seemed to live normal lives. Why should those with the Hashimoto’s variant be different?
Sadly, scientists are now finding that autoimmune diseases travel in packs.
If the immune malfunction of Hashimoto’s is not stopped, once it is done destroying the thyroid gland, there’s no predicting what it will attack next. In patients with one autoimmune disorder, the risk of getting other autoimmune conditions such as eczema, asthma, Hypothyroidism and rheumatoid arthritis (each being a condition where the body’s immune system attacks the skin, the lungs and the joints respectively) is far greater.
So if you have any of the clinical symptoms of an underactive thyroid and your standard labs come back with thyroid markers that are suspect, get your medical practitioner to check for Hashimoto’s thyroiditis before they simply prescribe that levothyroxine.
Learn how dietary supplements can help you get address the problem at its root and rescue the butterfly in your throat, so it can go back to keeping the rest of the body humming smoothly .
References:
Are Individuals With an Autoimmune Disease at Higher Risk of a Second Autoimmune Disorder? American Journal of Epidemiology Volume 169, Issue 6 Emily C. Somers, Sara L. Thomas, Liam Smeeth and Andrew J. Hall