
Fertility
Fertility Testing for Men and Couples Decoded
Jan 29, 2022Introduction
Infertile couples may have more than one cause for infertility. When planning a pregnancy, or trying to figure out the cause for infertility, your doctor may require both the male and female partners to run through tests.
While female fertility tests involve bloodwork to test hormones and ovulation, male fertility tests revolve mostly around semen analysis. In this article, we look at the various male fertility tests you might need to conduct.
Overview
In approximately 40% of infertile couples, the male partner is either the sole cause or a contributing cause of infertility[, according to an American Society of Reproductive Medicine survey.
Infertility affects men and women equally. Hence when planning a pregnancy, you might need to run through fertility tests for both partners.
Know more about female fertility tests in this detailed guide. Continue reading to learn about fertility testing for men and couples.
Fertility tests for men
Semen analysis is the first step in male fertility testing. This test simply requires examining a semen sample (produced via masturbation) under a powerful microscope. Tests revolve around the quality and quantity of sperm produced. This may be done at least twice at different times to ensure accuracy in results.
Usually, only a semen analysis is needed to diagnose male infertility according to a paper on the diagnosis of male fertility (in support of developing guidelines for WHO.
Semen analysis tests help determine various factors like:
1. Sperm quantity:
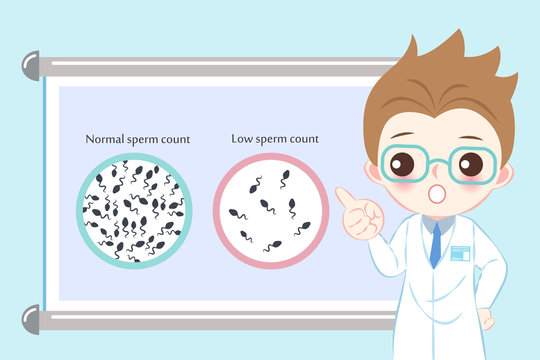
Sperm quantity refers to the number of sperm in a milliliter of semen. A normal sperm concentration is at least 15 million sperm per mL.
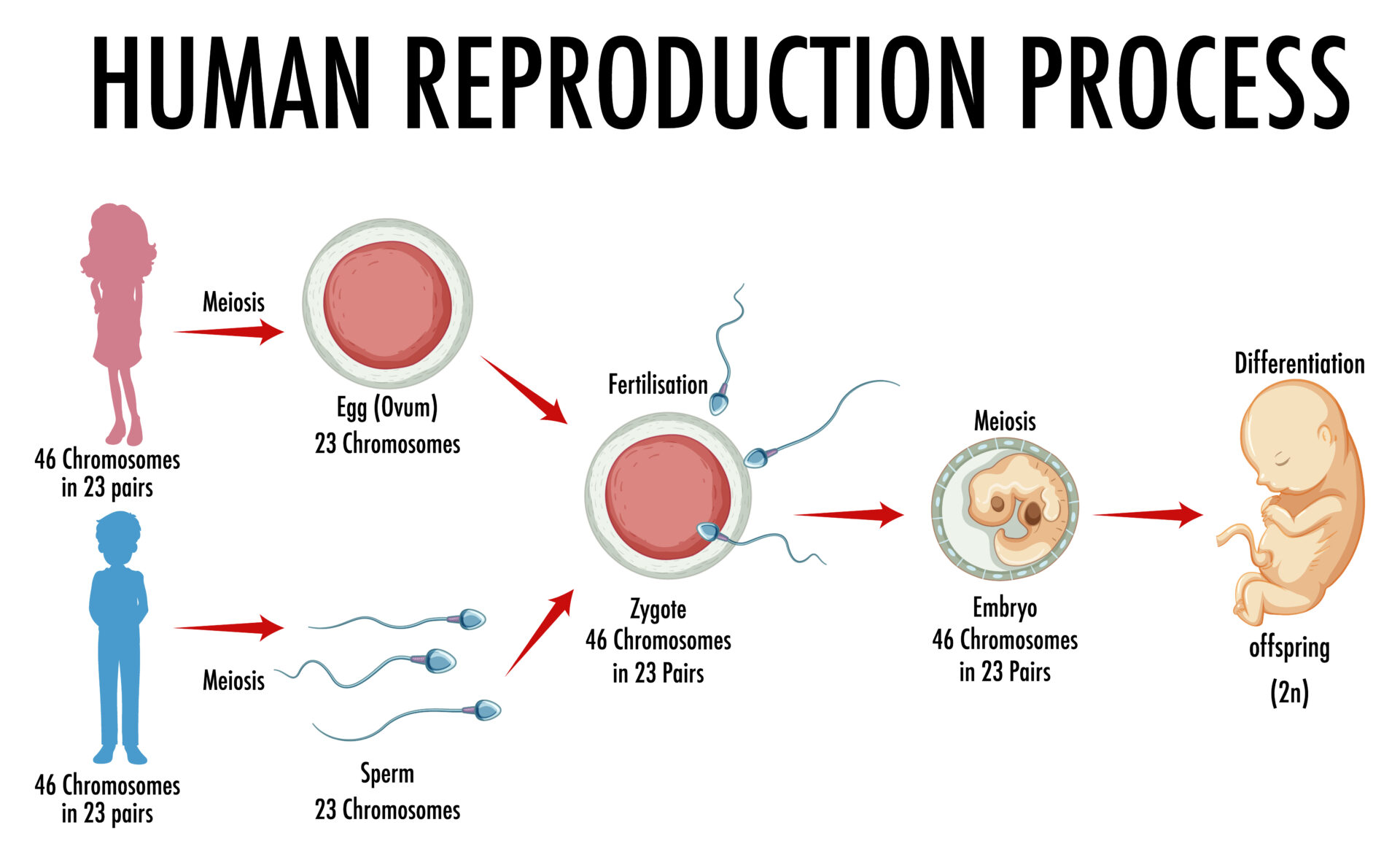
Out of these large volumes of sperm, just a few hundred actually reach the egg or the oocyte, due to various obstacles. Cervical mucus, getting stuck in the reproduction organs, etc., stops the millions of sperm a man releases from reaching the oocyte. Finally, out of the few that do reach the egg, it takes just one healthy, optimum sperm to fertilize the egg. That’s one big sperm lottery! Hence, higher the sperm quantity, better the chances of pregnancy.
2. Sperm motility
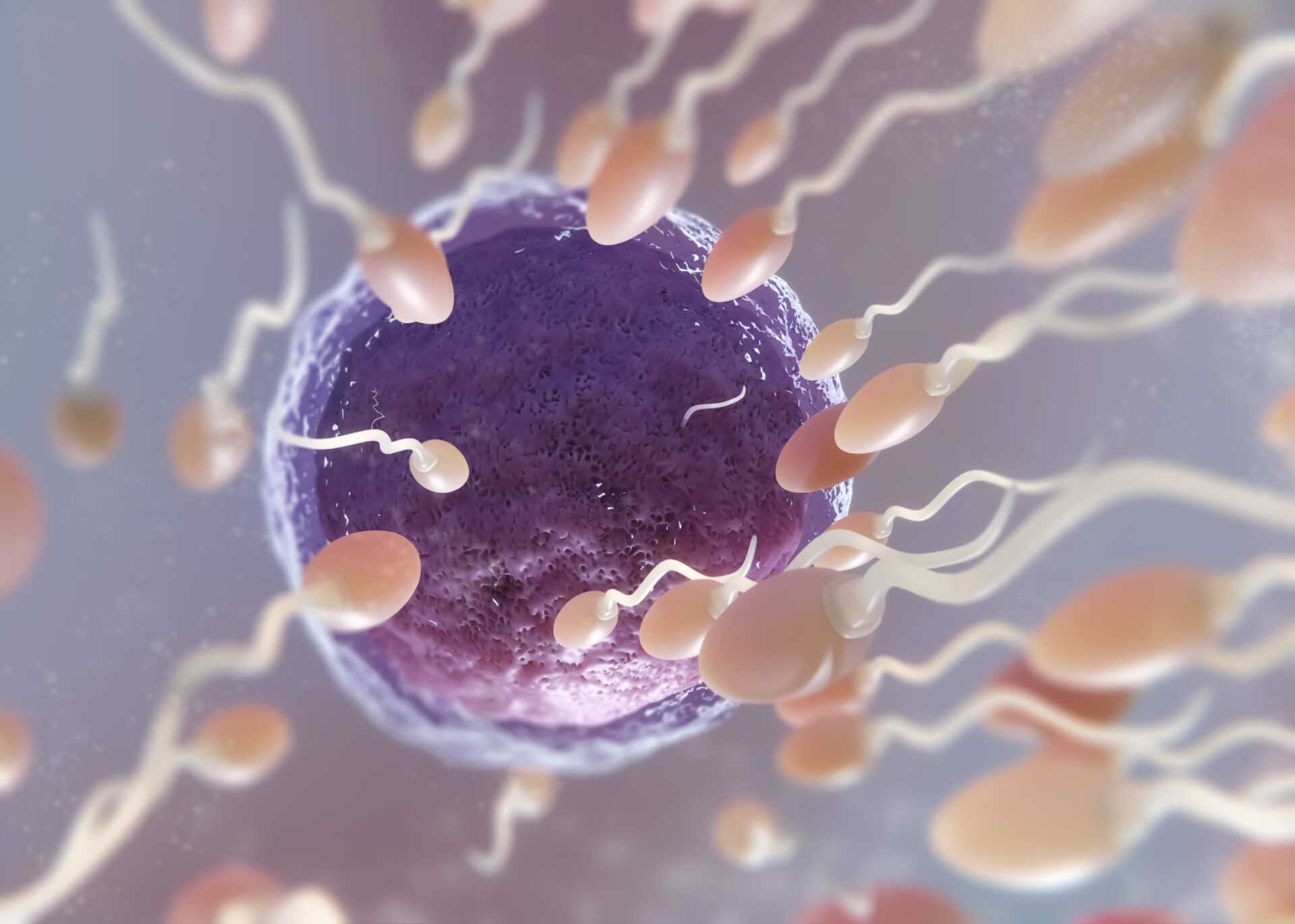
The sperms’ journey to female oocytes or eggs is propelled by flagellum on its tail. Sperm motility refers to the percentage of sperm that move in the best way to reach the egg. The speed and direction of movement determine whether the sperm can reach and penetrate the egg to fertilize it. At least 40% motile sperm is a normal result.
3. Sperm morphology (shape, size, and structure)
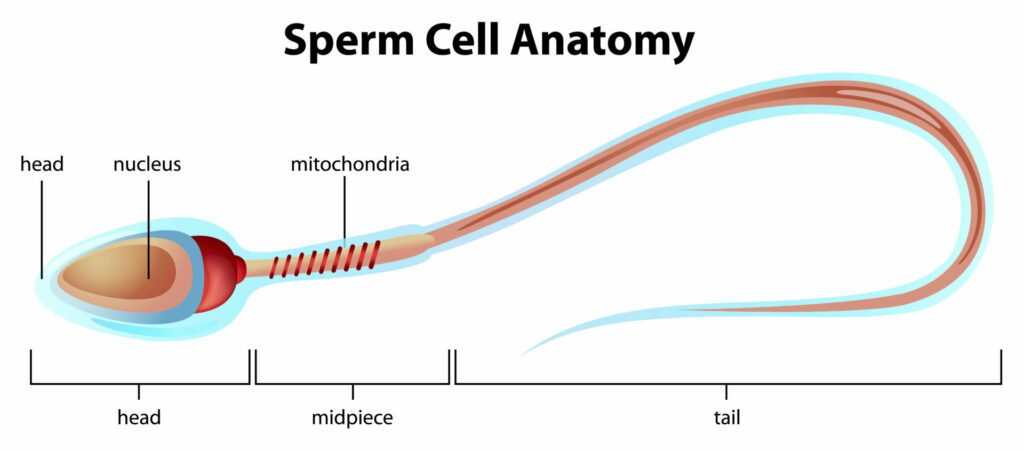
The sperm needs to have an optimal shape, size, and structure to be able to move forward and fertilize the egg. Morphology refers to the percentage of sperm that have the proper shape, size, and structure (also referred to as normal forms or NF). 4% NF or higher is a normal morphology result.
4. Semen volume

Checking the volume of semen ejaculated helps doctors find out any problems with the male reproductive system. While lower volumes don’t really affect fertility much, they can throw light on a blockage of ducts/ glands in the male system. Ejaculation less than 1.5mL is considered a low volume.
Male fertility testing can also involve evaluating the pH level and chemistry of the semen. Irregularities in semen pH or composition can pinpoint a defect in the testicles, such as an obstruction or infection.
Apart from semen testing and analysis, other testing performed to determine male fertility includes:
- A urologist may conduct a general physical exam including post-ejaculatory urinalysis (urine testing), to check for retrograde ejaculation.
- Doctors may conduct a DNA fragmentation test a.k.a. genetic testing of the sperm (looking for the presence of antibodies) and evaluation of immobile sperm (to see if they are dead or alive).
- You might have to bloodwork to check hormone levels, usually of FSH and testosterone, but sometimes also LH, estradiol, or prolactin
- The doctor may test for STDs (sexually transmitted diseases) during fertility testing.
- You may have to go through a scrotal ultrasound, to evaluate the seminal vesicles and scrotum.
- You can expect a testicular biopsy, which involves the removal of testicular tissue via a minor surgical procedure in case the doctor wants to check for testicular cancer.
- You may have to go through a vasography or a specialized X-ray, that is used to look for obstructions of the male reproductive organs.
Couple fertility tests

Certain fertility tests are carried out for both partners. Post-coital testing or PCT is one of these tests. PCT involves taking a sample of cervical mucus from the woman via a pelvic exam, several hours after the couple has sexual intercourse. It evaluates the interaction between the woman’s cervical mucus and the man’s sperm.
Genetic karyotyping or chromosome analysis is another test that couples may undertake. This blood test might help find the cause for your infertility or repeated losses. Knowing why you can’t get pregnant, or why you keep miscarrying, may help your doctor recommend the best treatment options.
Look at this detailed guide to know more about chromosome defects and genetic infertility.
At-home fertility tests
Fertility testing can be difficult or embarrassing for many people. That’s why the option of at-home fertility testing is also available. For instance, women can take at-home FSH (follicle-stimulating hormone) tests, while men can mail order sperm count test kits. These can be purchased online.
The downside with these tests is that they can’t fully evaluate your fertility and might not be very accurate. At-home FSH tests only detect high levels of FSH (if that is the case). At-home sperm count test kits, for example, only count how many sperm there are. They do not look at the other factors important in checking male fertility, mentioned earlier in this article. They do not provide any analytical information. Therefore, it is better to consult a doctor or a fertility specialist for your pregnancy-related troubles.
What Next after fertility testing?
The next step after testing involves consulting your doctor. Ask your doctor all questions that pop up during the process to get a clear idea of fertility testing. Never hesitate with your queries!
While reproductive system tests and subsequent treatments can be helpful in conceiving, most of the time, these lead to hormonal treatments and invasive procedures. These focus on solving the problem without delving into the root cause. So, if you are looking for less invasive, more natural methods that help you with infertility, you need to look at more functional and natural therapies.
‘Unexplained’ or ‘idiopathic’ infertility may be the diagnosis you receive, if all of the above reproductive system related tests turn out to be in the ‘normal’ range. This is where functional medicine shines.
Functional medicine looks into the root causes of infertility – causes that could often lie outside the reproductive system. For example, a lady with poor digestion could have poor fat and protein absorption, which in turn leads to less than optimal egg production. A man who is sleeping poorly and is under a lot of stress may have sperm that look normal, but are not strong enough to penetrate an egg and create an embryo. Functional medicine experts test for such unseen factors and address these root-causes of infertility.




