Basics
What Causes Type 2 Diabetes?
Nov 25, 2016Causes of Type 2 Diabetes
We all know the simplest way to check for diabetes is to see if you have too much sugar in your blood. This is most reliably measured by the HbA1c test, which measures how much sugar is coating your red blood cells on average over roughly 120 days. There are other tests too, that some doctors believe are better at catching diabetes earlier, at the prediabetes stage. When we ask “what causes Type 2 diabetes?”
we can answer this question in two ways. One, we can look at the factors that are known to increase the risk of diabetes and two, we can look at what actually happens in the body, as a mechanism, before you develop a type 2 diabetes diagnosis. Let’s look at both.
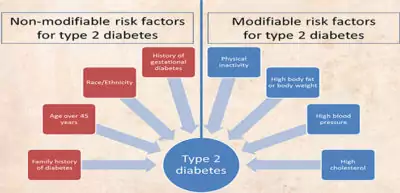
Risk Factors Associated with Diabetes
1. Genetics
If you have a close family member with diabetes, it increases your chances of developing Type 2 Diabetes significantly. Mind you, like all genetics, we know from research that this is not a dead end. ‘Epigenetics’ or how you live plays as important a role. You can greatly improve your odds of beating your genetics by living right.
2. Being Overweight
Obesity contributes a whopping 80-85% to the risk of developing type 2 diabetes. One of the mechanisms best understood for how being obese contributes to diabetes involves having too much abdominal fat, which leads to an “on fire” or inflamed state of your body. You can read more on this process later in this article. It is for this very reason that weight loss is one of the most effective ways of reducing diabetes risk and if you are already diabetic, of improving your diabetes control.
3. Having High Blood Pressure or Cholesterol
… are factors that contribute to the phenomenon called Metabolic Syndrome that is thought of as being the precursor to diabetes. There are several names and symptoms associated with this state.
4. Prescription Medications
Unfortunately, the medications that we take to save ourselves from other diseases may, if continued for a medium to long term, result in us developing Type 2 Diabetes. These medications include beta blockers and thiazides (Blood pressure lowering medications), corticosteroids (used for autoimmune diseases like asthma, rheumatoid arthritis, etc.) and statins (cholesterol-lowering medications)
5. Gestational Diabetes
If you’re a woman, this is relevant to you. If you suffered from diabetes during your pregnancy, it is called gestational diabetes and this can increase the risk of you developing Type 2 diabetes later in your life. There are some other medical conditions like polycystic ovary syndrome or PCOS that can be early indicators of diabetes that women should pay special attention to.
What Happens In Your Body Before You Get Diabetes?
Scientists are now saying that your body may be “on fire” for years before you develop diabetes.
Let’s break that statement down. Inflammation is the body’s repair response to damage or attack. It involves white blood cells and chemicals being mobilized to reach areas that need help. Like in the outside world, all response to attack is itself destructive in some way, so it should not go on infinitely.
Too much sugar is seen by the body as damaging. Once the damage is repaired the forces should withdraw, and the body should go back to homeostasis, or its “peaceful time.” But for some reason, in chronic diseases like Type 2 diabetes, the inflamed state continues for too long. Here’s why.
Sugar And Insulin: A Delicate Dance
Sugar is a necessary evil. It is needed for energy production in the body, and insulin is the key keeper that escorts sugar into your muscle cells for this purpose. But sugar is also inflammatory, so cells are very sensitive to how much they can handle in one go. Sugar can harm our cells, if there’s too much floating around at any given time.
When there’s too much sugar floating in the blood after a meal, (you ate that hi-carb meal, washed it down with a soda and went back to slump into your chair in front of the computer) the cells refuse to let insulin bring the extra sugar in. The result? Insulin production shoots up as the body tries to “muscle” the sugar into the cells. When the muscle cells don’t budge, excess sugar goes away into the fat cells, where it begins to accumulate.
Now stay with us for a moment here… this is where the plot thickens.
Insulin is itself inflammatory; that’s why too much of it, for too long, is bad. The body is meant to only have high amounts of it for short periods of time, after meals, to help push sugar into cells. After that, it is meant to go down nicely.
For reasons not yet clear to scientists, the fat cells don’t like insulin much either, and in their insulin-irritated state, they tend to have a nasty reaction to infections. So when we catch an infection (we all get the sniffles once in a while… or worse) the stage is set for the perfect storm.
The already irritated fat cells react badly to the infection, causing a disproportionate inflammatory (immune) reaction. And in this state, when insulin comes along every successive day, carrying more sugar to be stored, the fat cells freak out. They begin to stay inflamed like someone was stoking the fire all day long causes of type 2 diabetes.
Too much sugar = too much insulin = constant low-grade inflammation = diabetes in the long run.
This can cause serious damage to everything, including your brain. Citing a study in the New England Journal of Medicine, Dr. David Perlmutter, M.D., notes, “There is a significantly increased risk for cognitive decline with mild elevations of blood sugar, well below levels that would indicate diabetes.”
Adding Fuel to The Fire
Now multiply this by the number of times you do the things that also feed inflammation in the body: eat processed foods with tons of simple sugars, drink more than you should, stay stressed, don’t exercise, don’t sleep well, take inflammatory prescription meds…you get the idea. You keep stoking the fire until you have full-blown diabetes.
Now you get full blown symptoms of diabetes: feel tired all day (no sugar in the cells = no energy production, but they are too scared to let the sugar in), and you’re thirsty all the time (water is squeezed out of the cells to keep the corrosive sugar diluted in your blood, so you need more water). What’s more, none of your delicate organs like blood laden with sugar, so you may develop eye problems (diabetic retina damage), heart problems (congestive heart disease, or CHD), and tingling/burning sensations in your arms and feet (fine nerves are injured by high blood sugar too). These are the various complicated causes of type 2 diabetes
“When you spike your blood sugar level several times a day, every day, it is exactly like taking sandpaper to the inside of your delicate blood vessels,” says Dr. Dwight Lundell, M.D, world-renowned heart surgeon.
How to Put Out The Fire
While this is a highly simplified explanation, it’s clear that inflammation is what we want to reduce for type 2 diabetes prevention. And the key hormone that we want to have just enough of (not more, not less) is insulin.
So start by doing the basics right:
- Eat right.
- Sleep at least 6–8 hours a night (poor sleep is a huge risk factor for diabetes).
- Get the right amount of exercise.
- Find a stress outlet (yoga, deep breathing, meditation, or even sharing a good laugh with friends.
- Lose weight
Take the right supplements from Nature’s cabinet to keep your inflammation and blood sugar in control. Here is the ‘A’ team against diabetes—what works and why.





