Complications
Foot Ulcers: A Common Complication Of Type 2 Diabetes
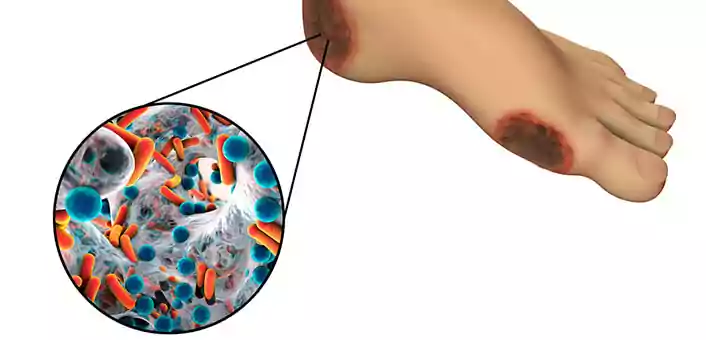
Feb 16, 2018Diabetic foot ulcers are responsible for more hospitalizations than any other complication of type 2 diabetes. In severe cases, diabetic foot ulcers may also lead to foot amputations. A diabetic foot ulcer develops as a result of a break in the skin. Due to high blood sugar levels, this wound is unable to heal itself. As a result, the wound goes deep, sometimes up till the bone. In fact, for diabetics, even a mild injury can develop into an ulcer.
Symptoms Of Diabetic Foot Ulcers
While an injury to any part of your body will initiate pain that will get your attention, in case of diabetics, things are a bit complicated. Due to neuropathy, diabetics usually lose sensation to the lower extremities. Any injury, therefore, goes unnoticed. Diabetic ulcers usually develop on the soles of the feet, and unless you specifically look underneath your feet, you wouldn’t notice the wound or injury. It is therefore important to identify early signs and symptoms of a diabetic foot ulcer. Some of these signs are:
- Drainage from your foot that stains your socks or leaks out into your shoe
- Unusual swelling
- Redness and irritation
- Odor from the feet
- Skin discoloration (black color)
- Callused area of skin
- Formation of a black tissue (eschar) surrounding the wound
- Odorous discharge from the wound
- Pain and numbness around the developing ulcer
There is inadequate (sometimes no) blood flow to the injury site. This leads to a death of the tissue around the ulcer. This can lead to a formation of gangrene due to infection of the site by opportunistic skin microorganisms.
Why Does A Wound Turn Into An Ulcer In Diabetics?
Slowed Down Healing Process
A wound occurs when the integrity of the skin is lost due to a mechanical injury. There is tissue damage as well as rupture of small blood vessels. Under normal circumstances, the body is capable of healing this damage by itself. In case of diabetes, the problem is compounded by high blood sugar levels, which slow down the normal healing process. The condition becomes worse with the slower ability of diabetics to sense a wound due to loss of sensation in the feet.
Poor Blood Circulation
Diabetics also have poor blood circulation in the legs and feet due to a condition called atherosclerotic peripheral arterial disease. In this condition, plaques (similar to those that form in the blood vessels supplying blood to the heart, leading to a heart attack) form inside the blood vessels in the legs and feet. These plaques, along with structural changes that occur in the blood vessels due to diabetes, do not allow adequate blood flow through the blood vessels. Poor blood circulation affects the transportation of vital nutrients and gas exchange (exchange of oxygen and carbon dioxide at the cellular level) to the tissues of the legs and feet.
Dry Skin
Dry skin is common in diabetics. This dryness may lead to cracking of the skin. Corns and calluses may also occur and all of these may cause bleeding wounds.
Risk Factors for Diabetic Foot Ulcers
- Neuropathy
- Poorly fitting footwear
- Poor hygiene
- Tobacco use (inhibits blood circulation)
- Insufficiently controlled blood sugar levels
- Walking barefoot
Tips For Preventing Diabetic Foot Ulcers
Avoid Walking Barefoot
Avoid walking barefoot as much as possible to prevent foot injuries. Becuase diabetics are very vulnerable to foot injuries, it is better to keep your feet covered at almost all times. Your doctor may recommend special diabetic socks and shoes to protect your feet. Socks may offer mild compression for enhancing blood flow to the legs and feet. Other foot-protective items for diabetics include casts, foot braces, compression wraps and shoe inserts (to prevent corns and calluses.)
Proper Foot Care Hygiene
Preventive care is important to avoid diabetic foot ulcers. This includes a proper hygienic routine that aims at keeping feet clean and managing proper blood sugar levels. You should wash your feet every day and look for signs and symptoms of injury. You should trim your toenails regularly. Always keep your feet dry and adequately moisturized. You can use a good quality moisturizing lotion. Change your socks frequently. Consult your doctor if you see any corns or calluses or changes to the skin that might seem abnormal.
Treating Diabetic Foot Ulcers
The primary aim of treating an ulcer is to stop its progression into a condition where amputation is required. Doctors can remove early-stage ulcers by a procedure called debridement or removal of dead skin, foreign objects or infections that may have caused the ulcer.
If the ulcer has been infected, the doctor may suggest an X-ray examination to assess the involvement of the underlying bone. Tissue samples of surrounding areas of the ulcer may be sent to a pathologist to find out the infecting organism. Once information on the infectious organism has been obtained, the doctor may prescribe supporting medication like anti-clotting and anti-platelet drugs.
The wound requires dressing that contains anti-infective medication like silver sulfadiazine, polyhexamethylene biguanide (PHB) and povidone iodine.
Surgical procedures may be required to help treat the ulcer in progressive cases. These help in eliminating the risk of further complications like amputations.
Final Thoughts
If you are a diabetic, you are prone to cuts, wounds and minor injuries to your feet that could easily develop into an ulcer. Regular inspection of your feet, proper hygiene and efforts to control blood sugar levels are the key to preventing foot ulcers and its further complications.




